Cervical osteochondrosis is a progressive dystrophic-degenerative lesion of the intervertebral discs in the 1-7 vertebral regions of the cervical spine.
Cervical osteochondrosis results in deformity, exhaustion, and then damage to the spinal cord. This disrupts normal blood supply and nerve conduction in the neck and areas innervated by the nerve roots of the cervical spine.
Cervical osteochondrosis can either be isolated or combined with other parts - thoracic, lumbar and sacral osteochondrosis.
Reasons
There are a number of factors that predispose to the development of osteochondrosis. These include:
- sedentary and sedentary lifestyle;
- types of sedentary work with a static load on the neck;
- overweight, insufficient physical development;
- dysplastic processes of connective tissue;
- circulatory disorders in the neck;
- neck injuries;
- scoliosis, poor posture, uncomfortable pillows and mattresses;
- hereditary predisposition, metabolic defects.
Symptoms of cervical osteochondrosis. Complications
The cervical spine is the most susceptible to the development of osteochondrosis. Its vertebrae are the smallest compared to other parts of the spine, the muscle frame is not very clear, and the weight of the head and the upright posture affect the spine. In the cervical spine, the vertebrae sit tightly together. Even a minimal change in them can cause the nerves and blood vessels to constrict and even move.
The most characteristic symptom that patients complain of is pain in the cervical spine. Depending on the affected area, the pain may be localized: in the clavicle and shoulder; along the cervical spine; on the anterior surface of the chest.
The first signs of cervical osteochondrosis may be insignificant: a feeling of heaviness in the head, headaches in the occipital region, pain in the neck in the evening, numbness or tingling in the shoulders and arms.
Leading symptoms
Vegetative-dystonic.
Severe "shooting" pain in the neck, in the area below the occiput. The pain occurs after staying in one position for a long time, after sleep, after constant tension of the neck muscles.
Difficulty moving the hand sideways, stiffness, numbness in the fingers. Neurological manifestations due to narrowing of the vertebral arteries are observed: headache, nausea, dizziness, unreasonable jumps in blood pressure.
Spinal symptom.
The pain is localized behind the left sternum.
This type of pain should be distinguished from angina pain (nitroglycerin brings relief with angina, but not in osteochondrosis).
With the gradual disruption of the structure of the intervertebral discs, they become compressed and the nerve roots are disrupted, as well as the narrowing or disruption of the arteries and veins passing through the region of the vertebral bodies.
This leads to the development of specific syndromes - radical and ischemic:
- defeat of the roots of the first cervical vertebra (C1): abnormalities in the occiput;
- C2 lesion causes pain in the crown and occiput region;
- C3 lesion causes pain in the neck on the affected side, decreased sensitivity in the tongue and hypoglossal muscles, speech disorders are possible;
- Damage to C4 and C5 causes pain in the shoulder and clavicle, decreased tone of the muscles of the head and neck, hiccups, respiratory disorders, and pain in the heart;
- C6 lesion is the most common, causing pain from the neck to the scapula, forearm, thumbs, skin sensitivity may suffer;
- C7 lesion - similar symptoms with pain in the neck, back of the shoulder, to the back of the hand, impaired arm strength and decreased reflexes.
Circulatory disorders due to constriction of blood vessels in the cervical vertebrae can cause headaches, migraines, dizziness, impaired vision and tinnitus, flickering of flies in front of the eyes, impaired autonomic function.
There may be manifestations of heart syndrome with excruciating pain, shortness of breath and palpitations, arrhythmias.
Complications.
Dislocation of intervertebral discs with the formation of a hernia (protrusion).
Rupture of the intervertebral disc with compression of nerves and blood vessels, possible compression of the spinal cord, which can be fatal.
Formation of vertebral bodies (osteophytes) of the spine with root lesions (radiculopathy), paresis and paralysis.
In case of the above complaints, it is necessary to contact an orthopedist or neurologist and conduct the necessary research.
Nutrition
Proper nutrition will significantly alleviate the condition with osteochondrosis. Nutrition should be complete. If a person has a normal body weight, you can take a therapeutic diet number 15, according to Pevzner. It contains all the necessary minerals and increasing amounts of fat and water soluble vitamins. You need to eat foods high in natural chondroprotectors. Chondroitin is found in red fish, animal tendons and cartilage, and chicken meat.
Be sure to take 1, 5-2 liters of clean water. Fluid is needed to prevent drying of the intervertebral discs.
Traditional and non-traditional methods of treatment
Treatment
Today, there are both traditional and non-traditional methods of treating osteochondrosis of the cervical spine.
Drugs of treatment: symptomatic therapy with analgesics to relieve pain; taking non-steroidal anti-inflammatory drugs to relieve inflammation and tissue edema; antispasmodics; drugs to improve blood circulation; chondroprotectors to restore the structure of the intervertebral discs.
This course of vitamin B group therapy, external agents for therapy - gels and ointments, creams with anti-inflammatory, warming and analgesic components.
It is recommended to wear a special collar (Shants collar) during exacerbation.
Complications of cervical osteochondrosis with intervertebral hernias that impair sensitivity and blood circulation can be treated immediately.
The duration of treatment depends on the severity of the condition, because osteochondrosis is a progressive chronic disease. Treatment can be long and lifelong prophylactic courses can be given.
Physiotherapy treatments.
These include exercise therapy, magnetotherapy, balneotherapy, laser therapy, acupuncture, Lyapko application therapy and massage.
Physiotherapy
For the treatment of cervical osteochondrosis, it is mandatory to exercise several times a day. These include stretching, self-massage, a number of special exercises. Avoid neck injuries and heavy loads.
Long-term sitting should be combined with periods of rest and warm-up.
The basis of cervical spine health is a strong and healthy back, physical activity, comfortable bed with anatomical pillows and mattresses, proper posture and proper nutrition.
Lyapko application therapy
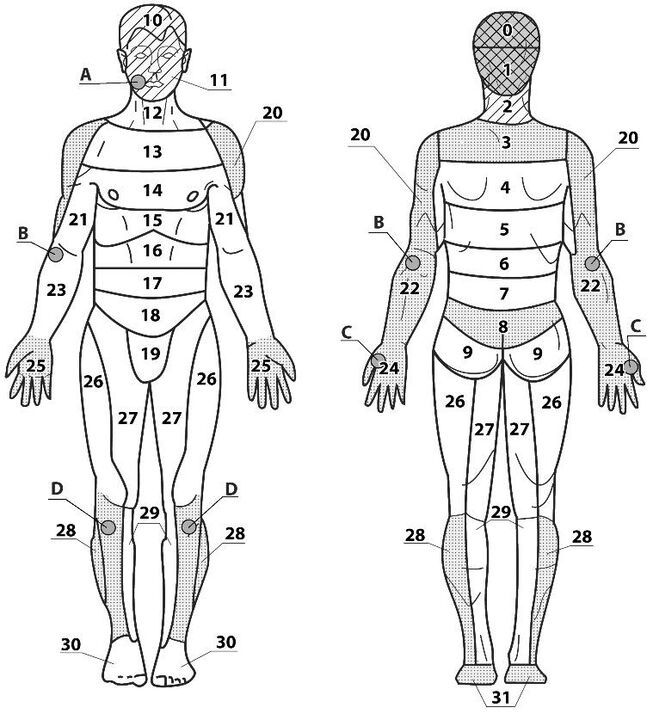
Areas of application:
- key 2, 3;
- additional 1, 4, 12, 13;
- assistant 20, 22, 28, 31.
General recommendations
When using the applicator, the main, additional and maximum pain zones are used, but in very severe pain, the applicators should be pulled above and below the painful zone, or the points and zones on the opposite side should be used. Exposure time 10-30 minutes.

If cervical osteochondrosis is combined with other parts - thoracic, lumbar and sacral osteochondrosis, application therapy can be applied to all parts of the spine simultaneously or in turn. The larger the exposure area, the better the effect.















































